© 2017
By Keith S. Wexler, MBA, Maternal Fetal Medicine, Prenatal Diagnosis and Biotech/Life Sciences Consultant, GENASSIST, Inc.
Paul Wexler, M.D., F.A.C.O.G., Medical Director, GENASSIST, Inc.
Clinical Professor, Department of OB/GYN, University of Colorado Health Sciences Center
Clinical Professor, Division of Genetics/Dept. of Pediatrics, Univ. of Colorado/The Children’s Hospital
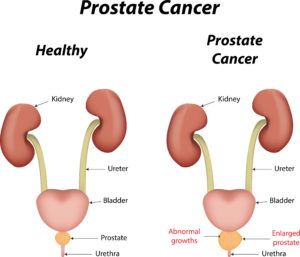
Prostate Cancer is the second most common cancer in men. Skin cancer is number one for men.
For many years Digital Rectal Examination (DRE) and blood Prostate Specific Antigen (PSA) was accepted as the best screening modality to be used in men, usually over the age of 50 years.
However, with the recognition in the variability in the course of prostate cancer, from rapid progression to little or no progression for many years, and the risk of both diagnostic and treatment approaches and false positive and false negative results, the use of PSA for routine prostate cancer screening has come under greater scrutiny.
Most urologists and the American Urological Association support the benefits of PSA screening for men between ages 55 to 70 years, at two year intervals, as outweighing possible risks.
Urologists also emphasize that PSA screening should not take place until the risks and benefits of the PSA screening are discussed thoroughly with the patient.
The American Urological Association did not recommend routine PSA screening in men under the age of 55 years or over 70 years.
Men diagnosed with probable Low Grade Prostate Cancer might be candidates for active surveillance rather than treatment. Some men with Low Grade Prostate Cancer might choose probable curative approaches despite the potential risks.
The availability of genomic testing for men diagnosed with Prostate Cancer or men at increased risk for Prostate Cancer might allow stratification of men into different risk and treatment strategies.
But at the present time genomic testing has not helped plot a course of monitoring and treatment of Prostate Cancer nor added to the use of standard parameters such as:
- Age of patient
- Grade of tumor
- PSA levels
- Stage of Disease
Magnetic Resonance Imaging (MRI) and an expanded MRI technique called Multiparametric MRI may allow earlier and more accurate diagnosis and more focused prostate biopsy and prostate tumor grading by helping clinicians to better distinguish between indolent from more aggressive tumors.
Possible chromosomes and genes associated with increased susceptibility to Prostate Cancer were identified as:
- Chromosome 8 (8q24)
- Chromosome 17 (17q)
- Gene *MSMB1- Chromosome 10 (10q11.2)
- Gene LMTK2 – Chromosome 7 (7q21.3-q22.1)
- Gene KLK3 – Chromosome 19 (19q13.33)
Gene HNF1B – Chromosome 17 (17q12)*The MSMB gene and closely associated gene NCOA4 is involved in Androgen Receptor Activity.



 © 2018, GENASSIST, Inc.
© 2018, GENASSIST, Inc.